The Deepening Crisis of Rural Hospital Closures in the United States: Will Montana’s Most Vulnerable Hospitals Be Next?
January 4, 2024
By Greg Gilpin
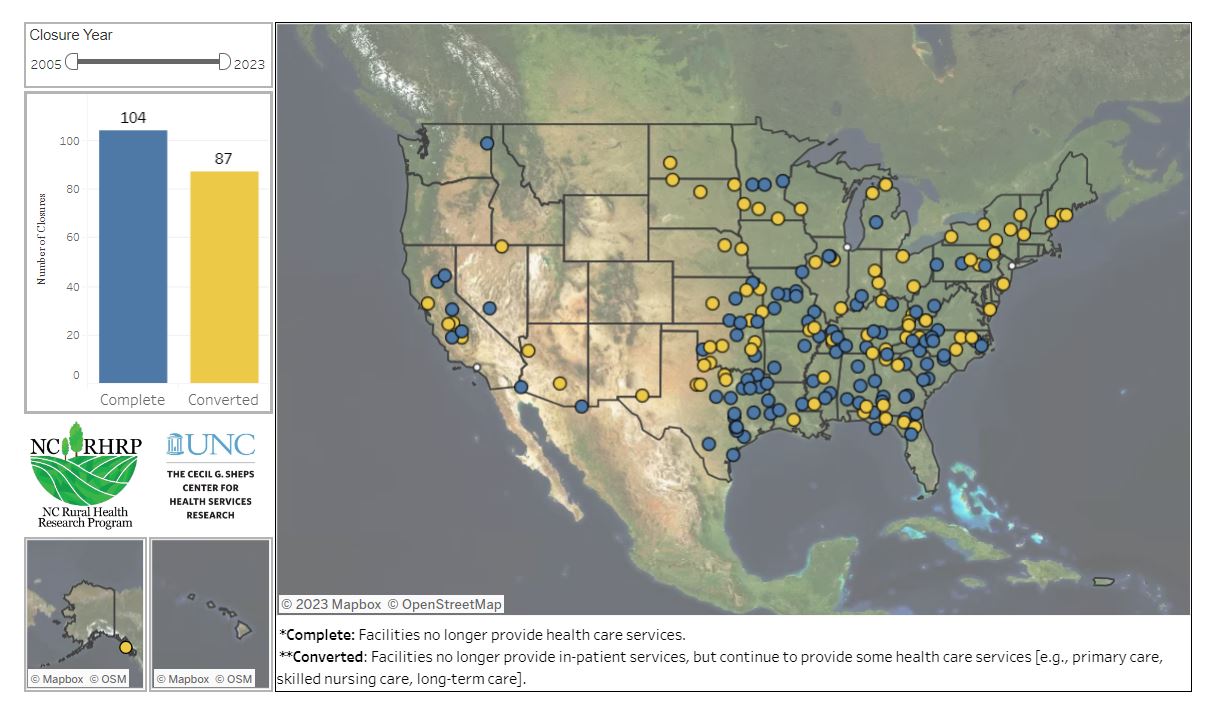
Rural hospital closures in the United States have become a significant public health crisis, with over 100 rural hospital closures and 87 conversions to urgent care facilities since 2005.1 These closures, driven by a complex blend of economic, demographic, and policy factors, have far-reaching implications not only for healthcare access but also for the broader rural economy. While none of Montana’s 55 rural hospitals have closed or converted, 64% have sustained loss of services and 25% are at risk of closing/converting within two years.2
Source: https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/
Financial Struggles and Demographic Shifts
A primary driver of these closures is financial instability, often rooted in low patient
volumes and high operational costs. Rural hospitals typically serve smaller populations
with a higher proportion of uninsured and underinsured patients, leading to significant
financial strain. This situation is intensified by the fact that rural populations
are often older and sicker, requiring more intensive and costly care. Studies have
shown that these economic challenges are a common thread in rural hospital closures
across the nation, including Montana.3,4
Impact of Healthcare Policies
Healthcare policies, particularly those related to Medicaid and the Affordable Care
Act, significantly influence the viability of rural hospitals. In states that have
expanded Medicaid, including Montana, there has been a noticeable reduction in the rate of rural hospital closures. This
is attributed to the increase in the number of insured patients and the higher rates
of reimbursement, which helps offset the cost of uncompensated care and private insurances
that tend to reimburse at lower rates.
While Montana has expanded Medicaid, recent redetermination of Medicaid benefits eligibility
post-COVID disenrolled nearly 93,000 Montanans. While 30% were found to be ineligible,
64% were disenrolled due to a failure to provide requested information. Several groups, including federal agencies and President Biden, have indicated that
Montana’s redetermination process requires streamlining and reduced administrative
burden. At the same time, the state has also increased Medicaid reimbursement rates. Without sufficient Medicaid funds, hospitals will continue to struggle financially,
leading to a higher risk of closure.5,6,7,8
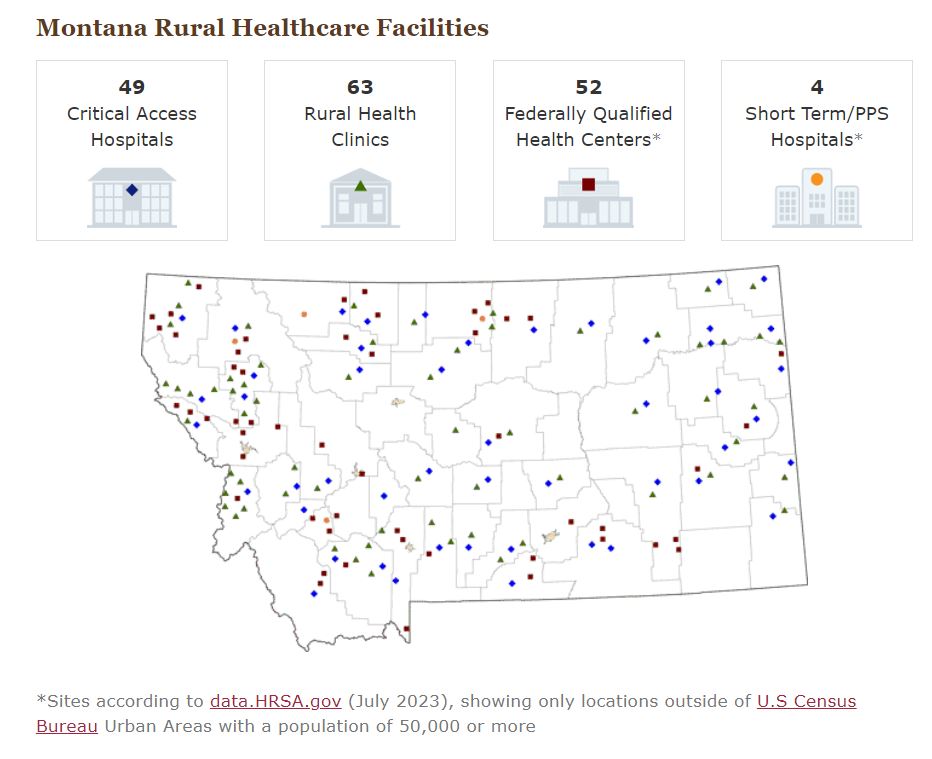
There are several Federal programs that are critical to maintain adequate funding in Montana’s rural healthcare facilities.
Source: https://www.ruralhealthinfo.org/states/montana
Critical Access Hospital (CAH) designation is given to eligible rural hospitals that provide essential services. The CAH designation reduces financial vulnerability and improves access to healthcare.
Rural Health Clinic certificate is given to eligible rural health facilities that provide primary care services. The certificate enhances reimbursement rates for providing Medicare and Medicaid.
Federally Qualified Health Centers designation is given to outpatient clinics that provide comprehensive, high-quality primary care and preventive services regardless of patients' ability to pay. The designation provides specific reimbursement systems under Medicare and Medicaid.
Short Term/PPS Hospitals designation through Centers for Medicare & Medicaid Services incentivizes less resource utilization per episode of care by reimbursing providers a pre-determined, fixed amount.
Montana's Unique Landscape
In Montana, the vast and sparsely populated landscape presents additional challenges
for rural healthcare. The closure of a single hospital can mean that residents must
travel farther distances for basic healthcare services. This is exacerbated by counties
that no longer have ambulatory services. This not only affects the timely delivery of care but also increases demand on surrounding
healthcare facilities as individuals to look to other providers for services. The
economic impact is also significant since hospitals often serve as one of the largest
employers in rural communities.9,10,11
Technological Advances and Potential Solutions
Despite these challenges, technological advances and innovative solutions offer hope.
Telemedicine, for example, has emerged as a vital tool in bridging the healthcare
access gap in remote areas. By leveraging technology, patients in rural areas can
receive consultations and care from specialists located elsewhere, reducing the need
for travel.12
Additionally, community-driven initiatives and alternative funding models are being explored to sustain rural healthcare. These include community health partnerships
and localized health programs tailored to the specific needs of rural populations.
The Way Forward
To effectively address the crisis of rural hospital closures, a multifaceted approach
is required. This involves not only policy reforms at the state and federal levels
but also community engagement and the adoption of innovative healthcare delivery models.
The goal is to build a resilient and sustainable rural healthcare system that can
withstand economic pressures and continue to serve the unique needs of rural populations.
Montana State University has several initiatives through the Office of Rural Health and Area Health Education Center. Additionally, through the Philanthropic gift of $101 million, Mark and Robyn Jones seek to address access to health care in rural and frontier
communities by expanding the supply of nurses and nurse-midwifery.
References
1The Crisis in Rural Health Care. Center for Healthcare Quality and Payment Reform.
2Rural Hospital Closures. NC Rural Health Research Program.
3Rural Healthcare into 2040 Trends, Challenges, and Opportunities. National Rural Health Association.
4 Kaufman et al. (2016). “The Rising Rate of Rural Hospital Closures.” Journal of Rural Health, 32(1), 35–43.
5Status of State Medicaid Expansion Decisions: Interactive Map. Kaiser Family Foundation, 2023.
6 “Redetermination challenges spur Medicaid coverage losses in Montana.” Health/Employee Benefits News.
7 “Montana Backs Away from Innovative Hospital Payment Model. Other Staes are Watching” KFF Health News.
9 Mills et al. (2023). The Impact of Rural General Hospital Closures on Communities—A Systematic Review of the Literature. Journal of Rural Health, 1-11.
10 Holmes, G. M., Slifkin, R. T., Randolph, R. K., & Poley, S. (2006). The Effect of Rural Hospital Closures on Community Economic Health. Health Services Research, 41(2), 467–485.
11 Alexander and Richards, "Economic Consequences of Hospital Closures," 2023.
12Rural Hospital Closures Threaten Access: Solutions to Preserve Care in Local Communities. American Hospital Association.

Greg Gilpin
Professor