RMHP3 Model and Goals
A Mental Health Preparation Pathway Designed for Montana
Need/Problem
Montana has three profound mental health needs that will be addressed by this project:
- One of the highest rates of death by suicide in the nation
- A growing set of challenges connected to drug abuse and addiction, and
- A serious shortage of rurally-prepared mental health providers.
Overall, we found that rural Montana schools are struggling to recruit and retain qualified mental health professionals. Additionally, mental health needs across the state continue to amplify, especially in relationship to youth suicidality and substance abuse.
Our Response
After further conversation and research, we determined in order to reach our most vulnerable populations, we will need to train, support, and deploy mental health professionals where they are needed the most; rural Montana.
Educators from Montana State University and the University of Montana engaged in a joint effort to explore the best way to meet these goals within their own education programs. We determined we could do more to help train and place mental health professionals in rural communities, starting in our own programs by expanding recruitment in rural Montana.Thus, the Rural Mental Health Practice/Preparation Pathway was born.
Our Model
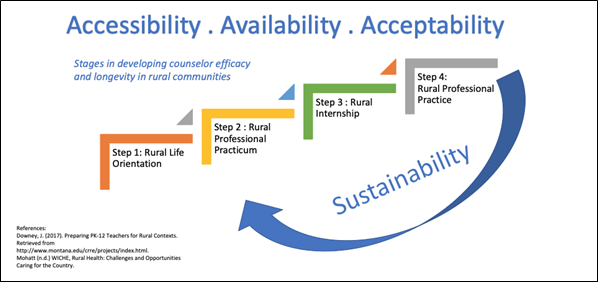
To address the needs of Montana, we proposed the Rural Mental Health Preparation/Practice Pathway (RMHP3) :
a cohort model where graduate counseling candidates serve in rural communities throughout
their program and their post-graduate prelicensure employment.
Accessibilitypresents a serious challenge for meeting the state’s mental health needs due to our massive geographic distances. To address issues of accessibility, RMHP3 will place graduate counseling internship candidates in schools and communities where distance makes access to mental health services the most challenging.
Availability highlights the lack of mental health providers working in rural areas. Rural mental health professionals tend to face large caseloads, significant isolation, and limited professional support due to the geographic isolation of their communities. RMHP3 will address the issue of isolation and limited professional support by utilizing a cohort model in which graduate counseling candidates will be supported by their peers.
Acceptability in this context refers to the stigma that can be associated with receiving mental health counseling. We are addressing these unique rural challenges to address stigma sensitively early in counselor development. Through their participation in the RMHP3, counseling candidates will be familiar with, and prepared to effectively respond to, rural families’ reluctance to seek treatment.
Sustainability is a fourth factor that will be addressed by RMHP3. Through the generation of a pathway from field experience to rural professional life, counselors who engage in this process will be prepared and motivated to remain in the communities in which they are placed.
 Rural Mental Health Preparation/Practice Pathway (RMHP3)
Rural Mental Health Preparation/Practice Pathway (RMHP3)
Intervention
We plan to meet our goals by establishing four Counseling Cohorts of ten (totaling 40 mental health professionals) from Montana’s Flagship Universities serving rural mental health needs in Montana’s high needs schools. In order to train our cohorts, we are using a 4 step process:
- Rural Life Orientation
- Rural Professional Practicum and Rural Counseling Course.
- Rural Internship and Online Learning Modules.
- Rural Professional Practice.
Short-Term Outcomes
Our short-term objectives are what we aim to achieve during our five year grant period. Our objectives include:
- Increase Partnership capacity with Montana State University, University of Montana, the Office of Public Instruction, public schools, communities, and School Based Mental Health providers.
- Prepare counselors with the necessary awareness, knowledge, and skills to address mental health needs sensitively and effectively in rural contexts.
- Expand University recruitment, preparation, and retention practices for rural students returning to their communities to practice.
- 40 counselors-in-training prepared to serve rural MT schools and communities.
Long-Term Goals
The long-term goals for this model are made possible through our model's focus on sustainability; by bolstering our counseling student's support and knowledge we are setting them up for success and the ability to maintain their position in a rural community. With sustainability in mind, our long-term goals are:
- Develop a model of best practice that prepares counselors-in-training to work in rural communities.
- Increased student and community access to fully prepared, high quality counselors.
- Counseling graduates are well prepared to address challenges of rural mental health.
- Increased networking and consultation available for rural mental health providers.
- 40 Mental Health Professionals employed and retained in rural MT schools and communities.
